Predictive placentas: Using AI to protect mothers’ future pregnancies
In partnership with UPMC, Carnegie Mellon researchers developed a machine learning approach for examining placenta samples to determine if mothers are at risk for complications in future pregnancies.
After a baby is born, doctors sometimes examine the placenta—the organ that links the mother to the baby—for features that indicate health risks in any future pregnancies. Unfortunately, this is a time-consuming process that must be done by a specialist, so most placentas go unexamined after the birth. A team of researchers from Carnegie Mellon University (CMU) and the University of Pittsburgh Medical Center (UPMC) developed a machine learning approach to examine placenta slides so more women can be informed of their health risks.
Source: Carnegie Mellon Engineering
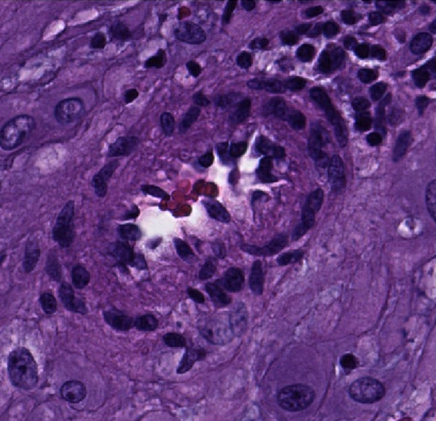
Machine learning can provide feedback about which cases would benefit from in-depth pathological inspection, like this sample revealing a decidual arteriole affected by early stage decidual vasculopathy.
One reason placentas are examined is to look for a type of blood vessel lesions called decidual vasculopathy (DV). These indicate the mother is at risk for pre-eclampsia—a complication that can be fatal to the mother and the baby—in any future pregnancies. Once detected, pre-eclampsia can be treated, so there is considerable benefit from identifying at-risk mothers before symptoms appear. However, while there are hundreds of blood vessels in a single slide, only one diseased vessel is needed to indicate risk.
“Pathologists train for years to be able to find disease in these images, but there are so many pregnancies going through the hospital system that they don’t have time to inspect every placenta,” former CMU Ph.D. student Daniel Clymer said. “Our algorithm helps pathologists know which images they should focus on by scanning an image, locating blood vessels, and finding patterns of the blood vessels that identify decidual vasculopathy.”
Machine learning works by “training” the computer to recognize certain features in data files. In this case, the data file is an image of a thin slice of a placenta sample. Researchers show the computer various images and indicate whether the placenta is diseased or healthy. After sufficient training, the computer is able to identify diseased lesions on its own.
It is quite difficult for a computer to simply look at a large picture and classify it, so the team introduced a novel approach where the computer follows a series of steps to make the task more manageable. First, the computer detects all blood vessels in an image. Each blood vessel can then be considered individually, creating smaller data packets for analysis. The computer will then access each blood vessel and determine if it should be deemed diseased or healthy. At this stage, the algorithm also considers features of the pregnancy, such as gestational age, birth weight, and any conditions the mother might have. If there are any diseased blood vessels, then the picture—and therefore the placenta—is marked as diseased.
“This algorithm isn’t going to replace a pathologist anytime soon,” Clymer said. “The goal here is that this type of algorithm might be able to help speed up the process by flagging regions of the image where the pathologist should take a closer look.”
This is a beautiful collaboration between engineering and medicine as each brings expertise to the table that, when combined, creates novel findings that can help so many people.
Jonathan Cagan and Philip LeDuc, Professors, MechE
This technology can decrease healthcare costs, allowing a majority of mothers and infants to have access to a microscopic placenta examination. The UPMC team provided the de-identified placenta images for training the algorithm; it would have been difficult to conduct this research without them. This kind of partnership is common at CMU. One of its most valuable assets as a research university is the level of collaboration that happens in almost every field.
“This is a beautiful collaboration between engineering and medicine as each brings expertise to the table that, when combined, creates novel findings that can help so many people,” said Jonathan Cagan and Philip LeDuc, professors of mechanical engineering at CMU.
“As healthcare increasingly embraces the role of artificial intelligence, it is important that doctors partner early on with computer scientists and engineers so that we can design and develop the right tools for the job to positively impact patient outcomes,” said Dr. Liron Pantanowitz, formerly the vice chair for pathology informatics at UPMC. “This partnership between CMU and UPMC is a perfect example of what can be accomplished when this happens.”
The paper, titled “Decidual Vasculopathy Identification in Whole Slide Images Using Multi-Resolution Hierarchical Convolutional Neural Networks,” was published in The American Journal of Pathology. This work was partially funded by the Center for Machine Learning and Health at Carnegie Mellon University through the Pittsburgh Health Data Alliance as well as the Office of Naval Research.
